Pain is one of the most common reason people seek care, yet it is commonly the least consistently managed. A certification training course suffering management can shut that void, translating standards right into dependable bedside technique. The greatest programs pair medical rigor with the genuine restrictions of ambulances, wards, facilities, and rehabilitation gyms. If you work in acute care, health care, paramedicine, nursing, physiotherapy, or allied wellness, developing skills in both analysis and intervention modifications outcomes promptly. I have actually seen it in my very own practice: fewer readmissions, shorter sizes of keep, and clients who finally rest via the night.
This guide walks through what a thoughtful pain management qualification resembles, just how to select a course that fits your setting and scope, and a functional path to be successful as soon as you register. Along the way, I'll discuss specialized choices like puaeme008 provide discomfort management for emergency situation -responders, pain monitoring programs for registered nurses and physio therapists, and brief courses hurting monitoring that slot into active rosters.
Why discomfort administration training is worth your time
Pain is not simply a sign, it is a motorist of problems. Unchecked sharp pain elevates catecholamines and can get worse cardiac ischemia, hinder air flow, and slow-moving mobilization. Inadequately taken care of chronic pain commonly spirals into deconditioning, mood problems, and polypharmacy. When clinicians complete a discomfort management training course that stresses analysis precision, multimodal therapy, and communication, the influence is quantifiable. On a surgical unit where we applied standard discomfort evaluations and daily analgesic optimization, the average time to first mobilization visited about a 3rd over one quarter. Client contentment scores rose, yet more notably, post-op lung problems fell.
A certificate signals to your group that you can structure treatment with intent, not behavior. It also assists in credentialing and advanced functions. Many companies now acknowledge a pain administration certification as proof of continuing capability, especially for broadened method registered nurses, scientific registered nurse specialists, and extended-scope physiotherapists.
What a solid certification course hurting management covers
The ideal pain administration training courses stay clear of the trap of being a pharmacology lecture stitched to a set of discomfort scales. They construct a functional structure you can use on a chaotic change, throughout a quiet ward round, or in a long speak with a complex patient. A full program typically includes:
Foundations of discomfort physiology and the lived experience. Expect protection of nociceptive versus neuropathic discomfort, peripheral and central sensitization, and how concern, sleep, and previous trauma improve discomfort handling. Good trainers attach theory to vignettes you'll in fact acknowledge, like the post-herpetic neuralgia person who enhances only after you deal with allodynia and sleep separately.
Assessment with nuance. Discomfort ratings are the beginning point, not the destination. You ought to practice useful goals, movement-based evaluation, and risk stratification for opioid-related damage. Pediatric, senior citizen, and cognitively damaged analyses must be more than a sidebar.
Pharmacological methods across settings. Short-acting versus long-acting opioids, opioid-sparing programs, neuropathic agents, ketamine for certain signs, and local anesthetic fundamentals. Search for material on secure deprescribing, kidney and hepatic dosing, and pharmacogenomic factors to consider where relevant.
Nonpharmacological and corrective strategies. Warmth, cold, TENS, pacing, rated direct exposure, mindfulness, and sleep health matter if they are delivered with framework and follow-up. Physiotherapists need to see rated motor imagery and desensitization techniques at work, not just on slides.
Communication that shifts outcomes. Pain is an arrangement, framed by depend on. Programs should educate scripting that confirms discomfort while setting practical targets, plus short treatments for catastrophizing and kinesiophobia.
Safety, equity, and systems. Naloxone co-prescribing, PDMP use puaeme008 provide pain management where applicable, handling opioid use problem without preconception, social safety, and access obstacles for country and remote people. For health centers, consist of acute pain service acceleration criteria and handover standards.
Documentation and metrics. If you can not measure your impact, you can not maintain it. Good training courses reveal you how to develop problem checklists linked to pain diagnoses, track feature, and utilize top quality signs that make it through an audit.
Mapping the training course to your role
You do not need every module at the very same deepness. Suit the program to your day-to-day decisions.
Nurses in severe care gain from limited assessment, PRN optimization, safe titration protocols, and nonpharmacological strategies they can supply at the bedside. Pain management training for nurses must consist of procedural analgesia support, delirium and discomfort differentiation, and acceleration formulas aligned with the facility.
Physiotherapists require durably used movement-based approaches. Pain management courses for physio therapists need to drill graded direct exposure, load progression, are afraid avoidance therapy, and methods to integrate analgesic timing with treatment sessions. In post-surgical rehab, understanding when to ask for a nerve block evaluation can save days.
Primary treatment clinicians and pharmacists require chronic discomfort frameworks. This consists of taper plans, rest normalization, perioperative opioid monitoring, and interprofessional recommendation standards for discomfort centers, psychology, and interventional specialties.
Paramedics and first -responders work under time stress. Systems like puaeme008 supply discomfort monitoring, commonly called puaeme008 provide discomfort administration within employment training plans, concentrate on instant assessment, safe management of analgesics in the field, nonpharmacological methods during extrication, and handover that preserves analgesic energy. If you operate in this atmosphere, select a program lined up with your territory's formulary and clinical practice guidelines.
Anatomy of a practical discovering pathway
A certification training course suffering management typically runs in mixed style. Expect self-paced understanding modules combined with workshops or substitute instances. Programs range from brief courses suffering management that take 6 to 12 hours, to even more intensive discomfort administration certification training courses that run 40 to 80 hours with analyses and instance logs.
I urge candidates to structure their research study around 3 arcs: assessment mastery, intervention fluency, and interaction under restriction. The material might look similar throughout programs, however sequencing issues. Practice analysis scripts with associates early, not after pharmacology. Find out to ask, after that to act, then to review.
Clinical exposure, even if substitute, does the hefty lifting. I have seen students enhance most after they present two or three longitudinal instances. One was a 58-year-old with fallen short back surgical treatment disorder, averaging 4 hours of sleep and strolling less than a block. After setting a two-week functional target, working with a neuropathic representative titration, and readjusting therapy timing, his six-minute walk improved by 60 meters and he reduced evening awakenings in fifty percent. The numbers were straightforward, the strategy was methodical, and the change stuck.
Emergency pain monitoring deserves its very own lane
Acute discomfort in the area and in emergency divisions has various dangers and possibilities. You commonly do not understand the baseline opioid exposure, comorbidities, or background of substance use, yet hold-ups compound suffering and issues. A concentrated emergency situation pain administration module stresses:
Rapid differential medical diagnosis of discomfort kinds on thin details. That consists of distinguishing time-critical conditions where analgesia should not wait, but the option of agent and route issues to prevent masking peritoneal signs or neurologic deficits.
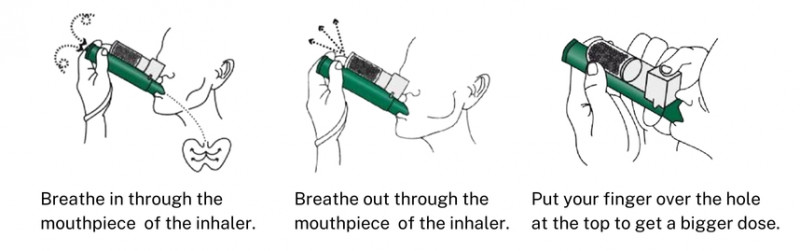
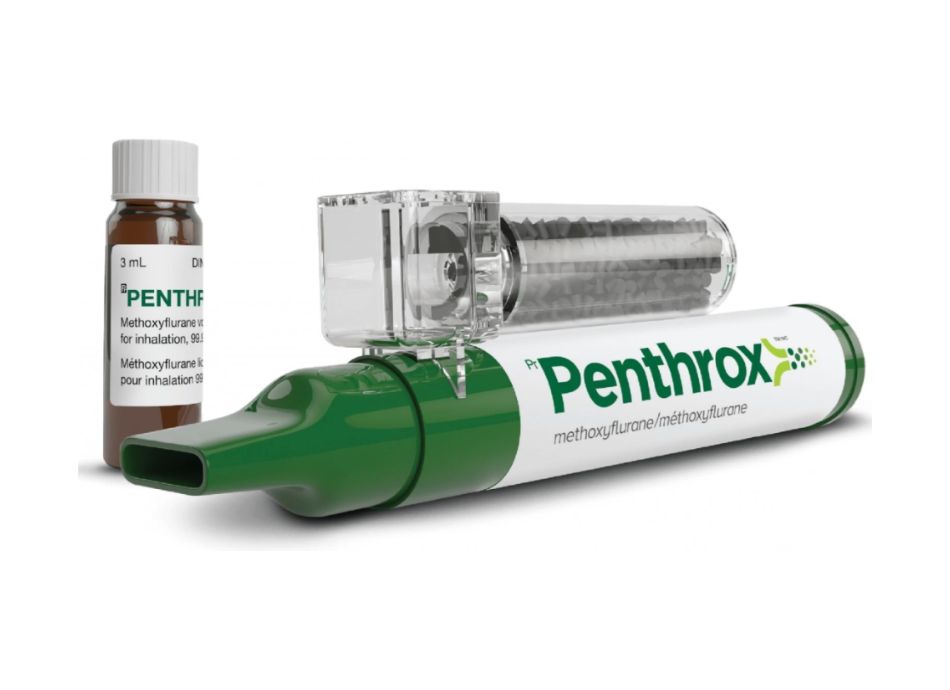
Analgesic pharmacology customized to prehospital and ED protocols. Breathed in analgesia, intranasal alternatives, IV titration with safety checks, and pediatric dosing that is very easy to calculate swiftly. Ketamine requires clear indications and contraindications.
Nonpharmacological techniques that purchase time and enhance end results. Splinting done properly, cold application, placing for dyspnea and pleuritic pain, and coaching breathing for severe anxiousness and panic where pain enhances distress.
Handover self-control. If you offer considerable analgesia in the field, handover should consist of timing, effect, and danger flags to avoid rebound pain or double dosing. Programs built around puaeme008 offer discomfort monitoring highlight this handover stringently.
I have actually watched brand-new paramedics, as soon as trained and monitored via a lots calls, lower time-to-analgesia by fifty percent without a single safety event. The difference was self-confidence anchored to procedure, not bravado.
Choosing among pain management training courses without obtaining lost
Marketing language looks comparable throughout suppliers. Kind programs by that developed them, how they evaluate you, and whether the web content straightens with your scope of practice. Integrity shows up in little information, like dosing modifications for kidney disability or case studies that consist of consent for nerve blocks.
You additionally want to see a plan for recurring competence. Some programs use a pain management certification training course with an one-time evaluation, after that recommend yearly refreshers. Others integrate in reflective practice and situation audits. If you prepare to keep a discomfort management accreditation that reinforces your resume, pick the latter. It will make your portfolio more powerful and your method safer.
Costs vary extensively. Short training courses might be budget friendly and concentrated, a good suitable for brand-new graduates or groups attempting to level up a single skill like neuropathic discomfort. Comprehensive pain administration training courses often justify higher charges with faculty accessibility, monitored method, and identified accreditation. Confirm what you obtain: downloadable devices, exam attempts, proctored OSCEs, and support for work environment projects.
The step-by-step course to qualification and impact
Here is a compact, sensible sequence that has actually benefited lots of clinicians I have mentored. It keeps momentum high and concentrates on modifications that stick.
- Clarify your range and setup. Provide the 3 most common pain circumstances you deal with weekly, and one risky circumstance you are afraid. This forms your program option and study plan. Pick a program that matches your territory and function. If you are in prehospital treatment, a program aligned with puaeme008 provide discomfort monitoring or your regional equal conserves translation work. Registered nurses must look for pain monitoring training for registered nurses with facility-specific escalation paths. Physio therapists need to guarantee there is considerable material on rated direct exposure, pacing, and pain education. Front-load assessment abilities. In the first two weeks, manuscript your history-taking, useful objectives, and threat stratification. Exercise on two patients and one colleague. Tape times and outcomes. Implement one change each week. Week one, adjust PRN timing and nonpharmacological assistances. Week two, present or optimize a neuropathic agent if shown. Week three, customize therapy sessions around analgesic peaks. Always track function. Build a little dashboard. Track numeric pain ratings just as context. Prioritize function: range walked, sleep hours, time to activate, or go back to work actions. Testimonial once a week and share with your preceptor or team.
This is the very first of both lists in this short article, purposefully short. Each product opens the next, and the last dashboard both verifies expertise and encourages doubtful colleagues.

Integrating pain management into team workflows
A certificate changes your practice, however the larger win is group uniformity. Discomfort administration programs that need a project part frequently ask you to carry out a small workflow renovation. The most effective candidates pick something noticeable and reversible, like a daily analgesia optimization huddle on a post-op ward, or a pre-physio analgesic timing procedure in rehab. Success depends upon:
Leadership that values little success. Beginning with a two-week pilot, then increase. If your pilot reduces the morning mobilization window by 15 mins throughout four people, your device has hours of performance obtained weekly.
Clear ownership. A single person updates the discomfort board, another causes escalation if targets are missed for 2 days, and a third audits regulated substance settlement. When no one has pain, discomfort owns the shift.
Data that informs a human story. A graph showing sleep hours and night-time pain along with quotes from the patient is influential. I have actually never ever seen a cosmetic surgeon neglect sleep recovered after 2 evenings of targeted adjustment.
Workflows need to additionally acknowledge side situations. Patients with chronic opioid treatment requirement different protocols. Those with unmanaged PTSD or high degrees of catastrophizing demand early psychology recommendation. Not every unit has these solutions in-house, so a well-constructed pain administration certification course need to help you build referral pathways and manuscripts for limited resources.
The pharmacology you will in fact use
A strong program equilibriums detail with energy. You need to leave able to do the complying with without grabbing a referral every single time:
Dose non-opioids proactively. Paracetamol and NSAIDs still bring the opioid-sparing load, but only if you make use of suitable schedules and represent kidney, hepatic, and bleeding threats. Several new grads underdose out of care that is unnecessary with proper screens.
Recognize when to choose an opioid, which one, and how to taper. Oxycodone, morphine, hydromorphone, and fentanyl each have particular niche advantages depending upon body organ feature and route availability. Prevent incorporating long-acting and short-acting opioids without a clear strategy. Support therapy to functional goals and day-to-day review.
Introduce neuropathic representatives with timelines that match fact. Gabapentinoids and SNRIs need days to weeks to reveal effect. Programs ought to highlight titration timetables, fall and sedation risks in older grownups, and techniques for discontinuation when they stop working to help.
Understand step-by-step and interventional choices sufficient to refer suitably. Area blocks and local anesthesia can be transformative post-op, yet timing and client selection matter. Physio therapists, particularly, benefit from understanding when to request a block evaluation to unlock early mobilization.
Use ketamine sensibly. Sub-dissociative application can be efficient for sure sharp pain circumstances, but requires clear procedures and monitoring. Good training programs show both potential advantages and the behavior side effects that agitate individuals and team when unanticipated.
The aim is not encyclopedic recall, it is safe and crucial action when your client is in front of you.
Communication and expectation setting
Pain monitoring is 50 percent pharmacology, 50 percent discussion. You will certainly discover to state things that shift an individual from a numeric target to a useful one. Instead of encouraging zero pain, you might supply consistent gains: walk to the mailbox, then around the block, then to the park. This reframing decreases distress and reduces the chase for rising dosages that let down everyone.
For families, scripts assist when pain lingers regardless of best efforts. Explain the strategy, side effects to look for, and what improvement will certainly look like day by day. In one clinical ward, giving a one-page pain plan that included convenience measures family members can assist with cut call bell use over night and better mood on both sides of the bed.
Cultural safety sits inside interaction. Discomfort expression differs across societies and individuals. Training ought to instruct you to ask open inquiries, stay clear of presumptions regarding stoicism or overestimation, and engage interpreters early when language obstacles exist.
Assessment pitfalls and how good programs show you to stay clear of them
I have seen 2 typical mistakes in medical professionals before added training. First, overreliance on a single numerical rating. Second, failing to reassess. A pain rating without context can misinform, especially in older grownups with delirium or in patients who underreport to prevent being labeled. The repair is easy and teachable: set the score with workshops for pain management certification a functional objective and a concentrated exam, after that reassess at predictable periods after an intervention. Many certificate programs require you to send two reassessment notes per case, a behavior that sticks.
Another risk is the one-size-fits-all analgesic. If your default is a solitary opioid, you will certainly overuse it. Multimodal regimens that value renal function and step-by-step context are much safer and frequently much more efficient. An organized discomfort administration program need to present counterexamples that test reflexes and offer a far better algorithm.
Assessment, certification, and maintaining competence
Pain monitoring certification usually includes on the internet quizzes, case-based short solutions, and, in the stronger offerings, observed structured professional examinations. I discovered most from OSCE stations that required me to negotiate goals with a standardized individual while explaining dangers of opioids and establishing a clear prepare for the following 48 hours. If your program provides optional OSCEs, take them.
After you earn a pain administration certification, prepare for refresher courses. Drug formularies alter, and so do guidelines for opioid usage, naloxone circulation, and perioperative treatment. The most defensible method is to complete a brief upgrade every 12 to 24 months. If your method consists of emergency situation treatment, seek modules aligned with upgraded scientific method guidelines similar to those embedded in puaeme008 provide pain management.
Keep a small portfolio: a log of challenging instances, your audit results on function metrics, and representations on at least two cases where your strategy altered mid-course. This is what transforms a credential right into a specialist asset.
Special tracks for nurses and physiotherapists
Pain management training for registered nurses ought to concentrate on three layers: precise assessment, protocol-driven titration, and nonpharmacological assistances registered nurses can provide without delay. Programs that consist of simulation for tough conversations function well, particularly for tapering requests or taking care of family members expectations. Registered nurses typically come to be the champions of day-to-day analgesia optimization, which is where the largest gains hide.
Pain administration courses for physiotherapists should push beyond education and learning into rated exposure that is measurable. I have seen therapists transform a client's outlook with a six-week strategy that balances tons and worry. Programs that require therapists to send pre and post practical metrics raise the requirement. When specialists and nurses line up, the morning home window, about one hour after analgesia, ends up being a trusted system for progress.
Short training courses versus comprehensive certification
Short programs suffering management have their location. For teams needing a quick tune-up or to systematize a single practice modification, a focused 6 to 8 hour training course is warranted. Use them to boost pediatric application safety and security, to turn out a new nonpharmacological toolkit, or to tackle neuropathic discomfort options.
A complete discomfort monitoring qualification course is much better if you prepare to be a go-to source or to lead high quality improvement. These programs offer you breadth, supervised method, and an assessment that stands in efficiency reviews. In numerous systems, such a certification supports applications for innovative positions or portfolio pathways.
A portable preparedness checklist prior to you enroll
- Define your result: promo, role expansion, or much better individual circulation on your unit. Confirm placement: does the course match your medicines, protocols, and reference networks? Secure time: block shielded slots for study and two medical instances to apply learning. Arrange mentorship: a teacher or senior clinician that will certainly examine your cases. Plan your audit: choose one practical statistics you will track for four weeks post-certification.
This second and final checklist keeps you honest. When clinicians complete these actions, they are even more likely to execute change rather than soak up content and wander back to old habits.
What success looks like six weeks after certification
Gauge success on the ground, not in the frame on your wall. On a medical flooring, look for earlier mobilization, less nighttime calls for development discomfort, and much shorter lengths of remain in uncomplicated situations. In health care, search for less early refill demands, more regular practical gains, and much better sleep reported at follow-up. In prehospital care, display time-to-analgesia, unfavorable occasions, and handover quality notes.
I worked with a regional group that combined a certification training course with a single workflow change: an everyday testimonial of people whose rest was disrupted by pain. Evening registered nurses applied a conventional nonpharmacological protocol and intensified targeted adjustments in the morning. Within a month, the system reduced wakeful evenings associated with pain by approximately a quarter, and daytime therapy sessions ran closer to arrange. None of this required brand-new medications. It needed a common language and a plan.
Final thoughts from the center floor
Pain will always be a moving target, shaped by biology, psychology, and context. A discomfort monitoring certificate gives you extra arrows in the quiver and the judgment to select the ideal one under stress. If your path indicate emergency pain administration, align your training with certified systems like puaeme008 give discomfort administration. If you lead on a ward or in a center, take into consideration a comprehensive pain administration qualification that includes top quality renovation and instance supervision. Registered nurses and physio therapists will certainly discover devoted courses that develop the devices they make use of daily.
The actual mark of success is not the certification itself, but a person who informs you they can ultimately dress without help, stroll their canine, or sleep without anxiety of the evening. That is what this training is for, and it is within reach when coursework converts right into constant practice.